8.1 Degenerative Diseases of the Spine
This is a significant chapter, as degenerative diseases of the spine are a socio-economic issue, either in young or in aged population.
The incidence of these diseases is growing. Aged people do not tolerate any longer to be "invalidated" by spinal back pain. Most of these diseases are of orthopedic or physiatric interest. The following is a series of diseases of neurosurgical interest, although "overtreatment" is around the corner.Clinically, they present with irradiated pain, neurological deficit in the territory of the involved nerve, paraparesis or tetraparesis if the cord is compressed.
Diagnosis is made on CT Scan and MRI. Dynamic plain radiographs should always be done to exclude spine instability.
This condition is due to ligamentous hypertrophy, associated with arthrosis and cervical disc rigidity. The result is narrowing of the space for the spinal cord in the canal, as well as of the space for the nerves in the foramina. Cervical stenosis may be very disabling, as it causes severe pain and neurological deficit of the upper and lower limbs, with spasticity that may become severe.
Posterior laminectomy with or without stabilization is the therapy of choice for symptomatic cervical stenosis. Sometimes, an anterior approach (as in the case of cervical disc disease) may be more indicated.
It is the same disease at the lumbar level and a little more frequent. As in the case of cervical stenosis, it is prevalent in the aged population.
At the lumbar level, there is no more cord. The compression is on the spinal roots that get out from the spine to form the femoral and sciatic nerves. Patients with spinal lumbar stenosis typically have pain while walking. The pain improves while sitting or laying down. The pain may be severe and disabling, as the patient can walk only for few minutes.
In obese patients, the first therapy is diet.
Neurosurgery has the same role as for cervical stenosis. With correct indication, posterior laminectomy with or without internal stabilization gives quite good results in terms of quality of life.
A herniated cervical disc may cause spinal cord and spinal root compression. Thus, the symptoms may be severe: pain to an upper limb, neurological deficit related to the affected root/roots, paraparesis and spasticity if the cord is compressed (Fig. 8.3). Neurosurgery is useful, if conservative therapies have failed, and mandatory in cases with severe and/or progressive neurological deterioration. Manipulations are contraindicated in cases of herniated disc.
Herniated cervical disc surgery is performed from the anterior route in the neck, with the operating microscope. It is an elegant and refined operation. The disc is removed and replaced with an articulated prosthesis (arthroplasty), in younger patients to preserve the mobility of the affected segment, or with a fixed prosthesis (arthrodesis).
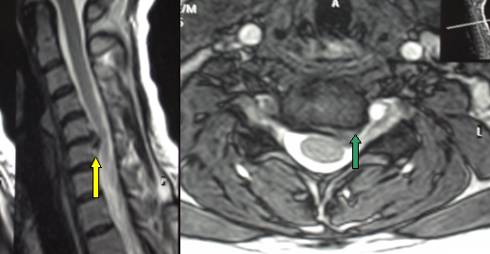
Fig.8.7: Lateral MRI view of a typical monosegment (C5-C6) herniated cervical disc (yellow arrow). On the right, axial view showing the herniated fragment (green arrow) which compresses the left C6 root.
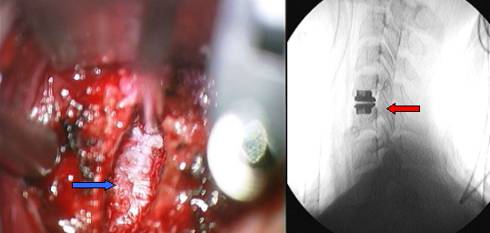
Fig.8.8: Intra-operative view under magnification with the operating microscope after disc removal. The blue arrow points to the anterior surface of the spinal cord with its intact dura. On the right, radiograph taken after insertion of an articulated prosthesis (red arrow).
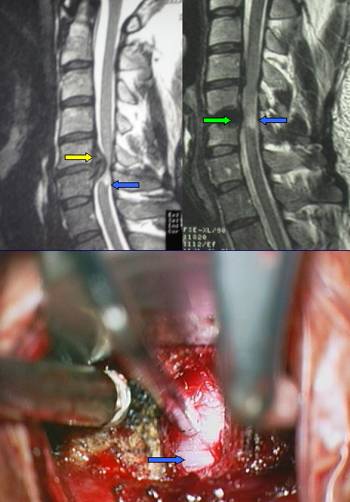
Fig.8.9: Very large herniated C5-C6 cervical disc (yellow arrow) with major spinal cord compression. The blue arrow points to spinal cord damage. Top right, post-operative MRI: the green arrow points to an artifact due to the fixed carbon implant; the spinal cord has recovered its normal profile, although retaining signs of anatomical damage. Bottom, intra-operative view under the operating microscope; the blue arrow points to the anterior surface of the spinal cord. In cases with severe spinal cord suffering, the best choice is an arthrodesis (fixed prosthesis).
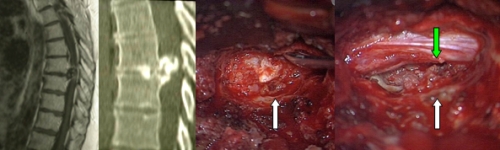
Fig.8.10: On the left, MRI and CT Scan pictures of a very large symptomatic thoracic herniated disc (D7-D8). On the right, operative view through the extrapleural, costotrasversectomy approach. The white arrows point to the herniated disc and the cavity after removal (right); the green arrow points to the spinal cord returning to its normal position.
Diagnosis is made on the basis of MRI and CT Scan images. Obesity is a bad prognostic factor. If symptoms persist for several weeks, microneurosurgical removal is the therapy of choice. If the indication for neurosurgery is correct, results are quite good.
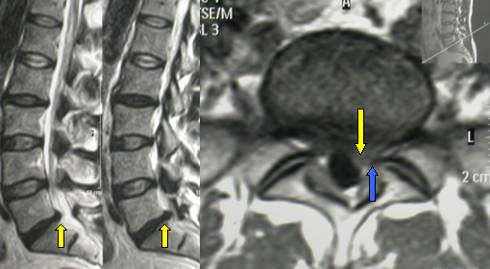
Fig.8.11: MRI of herniated lumbar disc at L5-S1 (yellow arrows). On the right, in axial view, compression of the root (blue arrow) by the herniated disc (yellow arrow).

Fig.8.12: Intra-operative view under the operating microscope. The size of the field is about 2 cm. From left to right: suffering S1 root (blue arrow); herniated disc (yellow arrow); root after disc removal (blue arrow).
Page 31



 Spinal Tumors
Spinal Tumors Previous Page
Previous Page