This is the most frequent glioma. Just as other brain tumors, it is classified on the basis of its malignancy into: low grade (
WHO grades I and II); relatively benign; and high grade (
WHO grades III and IV). Grade IV is the most malignant one and also defined as
glioblastoma multiforme (GBM).
A special kind of this tumor is
pilocytic astrocytoma. This is a grade I tumor, benign and generally resectable, if its location is favorable. It is the most frequent in childhood (cerebellar and temporal locations). It may also be located in critical areas: hypothalamus, brainstem; the removal in these cases is technically challenging.
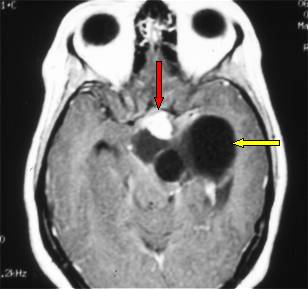
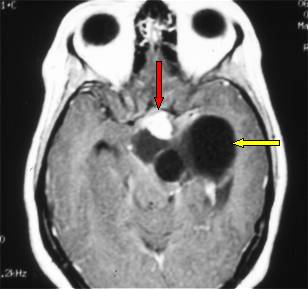
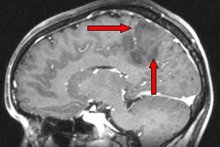
Fig.5.1: Cystic pilocytic astrocytoma of the
hypothalamic region. The yellow arrow points to its cystic part, the red one to the solid part.
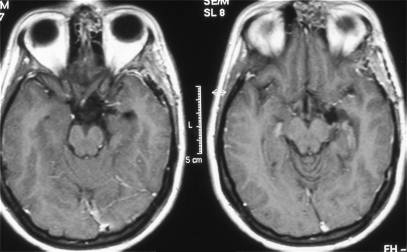
Fig.5.2: Post-operative image of the same case with total removal of the tumor, despite its difficult location.
Pilocytic astrocytomas grow slowly and are clinically evident with intracranial hypertension and hydrocephalus when located in the cerebellum or brainstem, and seizures when located in the cerebral hemispheres. They generally have a large cystic part. Surgery of these tumors must be carried out in qualified centers with the use the most advanced operative and monitoring technologies.
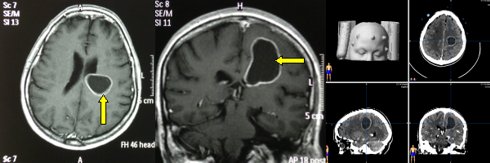
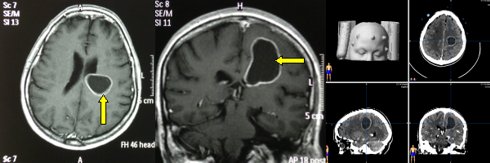
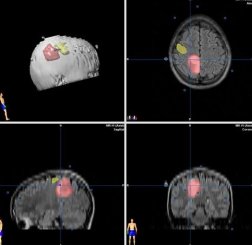
Fig.5.3: Deep left parietal cystic pilocytic astrocytoma (yellow arrow). Right: surgical planning with the
neuronavigator combined with
CT Scan.
It has some subtypes: fibrillary, gemistocytic and protoplasmatic astrocytoma. This subdivision is rather irrelevant from a clinical point of view. Low-grade astrocytomas grow slowly, but can infiltrate the surrounding brain tissue, sometimes diffusely (gliomatosis).
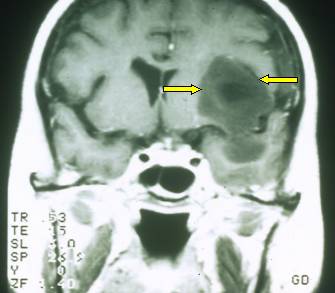
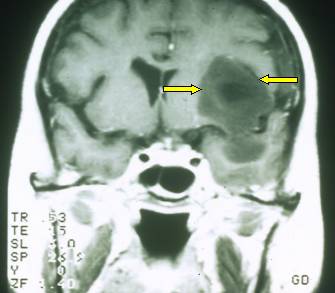
Fig.5.4: Left fronto-temporal low-grade astrocytoma. It is the dark grey dumbbell area (yellow arrow). The location is critical for language and motor functions.
Low-grade astrocytomas may cause partial and/or generalized
seizures (
see Figures 4.1, 2, 3) and may be complex if their location is temporal or deep temporal.
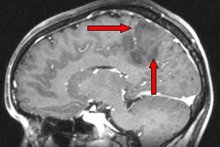
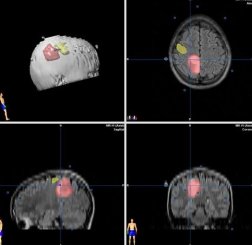
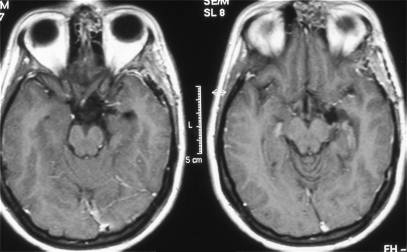
Fig.5.5: Left - the red arrow points to an area recalling a low-grade astrocytoma; right - surgical plan at the neuronavigator; the tumor is in red, the motor area in yellow.
Diagnosis at
MRI may be difficult. These tumors do not enhance after contrast administration. The lesion may be confused with inflammation, multiple sclerosis and scars secondary to old vascular lesions.
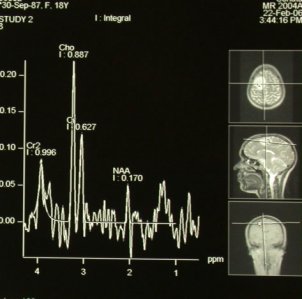
Spectroscopic MRI may be of help, as it identifies the biochemical component of the tumor.
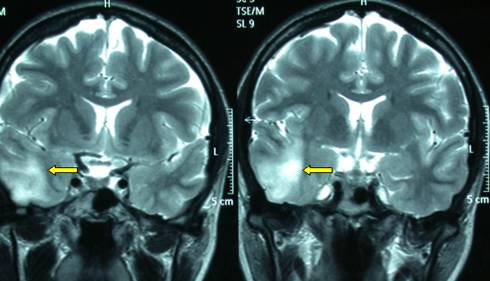
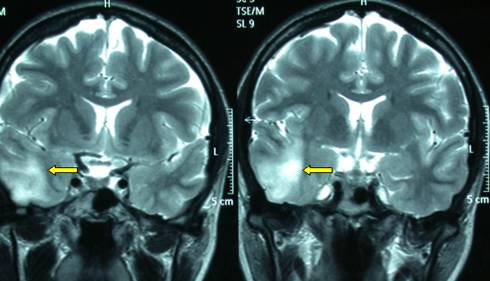
Fig.5.7: This
MRI shows a right temporal pathological area (yellow arrows), difficult to diagnose. Upon surgery, it turned out to be a low-grade astrocytoma.
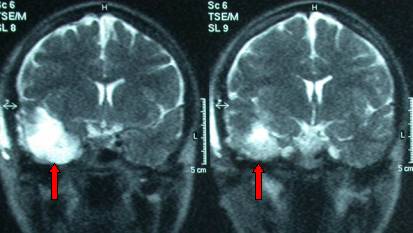
Fig.5.8:
MRI of the same case after surgery. The residual cavity is shown by the red arrows.
should be removed; the larger the removal, the better the result in terms of survival. This is feasible in non-critical locations. Currently, even tumors in critical areas may be operated upon thanks to adequate pre-operative planning and intra-operative monitoring (
functional MRI,
neuronavigator, Brain Mapping). Some patients may be operated even in the awake state, to minimize the risks of damaging language areas or the motor cortex and tracts. The patient and the monitors alert the surgeon during the operation.
Nevertheless and despite apparent "radical removal", astrocytomas regrow, generally as more malignant. Their recurrence may occur after many years. In patients undergoing "gross total removal" and not showing any residual tumor upon post-operative MRI, radiotherapy and chemotherapy may be done at a later stage. Correct antiepileptic medication may be crucial to a good quality of life for these patients.



 Glioma
Glioma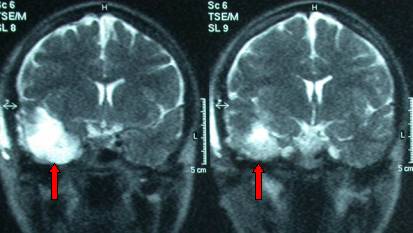
 Previous Page
Previous Page