It constitutes 2-3% of intracranial tumors, 5-13% of pediatric intracranial tumors. 60% of craniopharyngiomas occur in adult age. These tumors grow in the sellar region and in the third ventricle. Although benign, they have strong adhesions to the surrounding nervous structures: chiasm, stalk, hypothalamus. They are frequently cystic and may be very large. Pituitary function is generally impaired; optic nerves and chiasm are severely compressed. In children, they may cause growth impairment. If very large, they may cause hydrocephalus and intracranial hypertension.
The diagnostic tools are, as usual, CT scan and MRI.
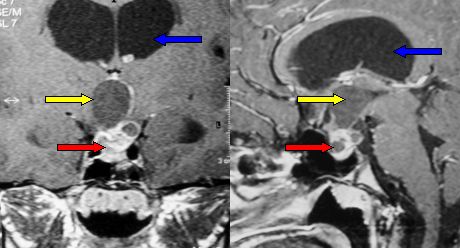
Fig.5.42a: Typical craniopharyngioma at frontal and lateral MRI scan. The yellow arrows point to the cyst, the red to the solid part of the tumor and the blue to a dilated lateral ventricle (hydrocephalus).
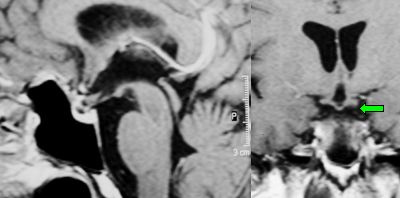
Fig.5.42b: Same case as in Fig. 5.46 after complete removal with a mininvasive supraorbital approach. The green arrow points to the optic chiasm.
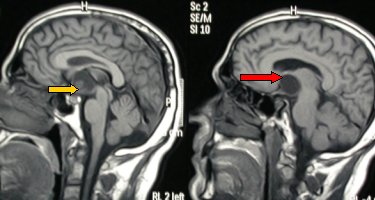
Fig.5.43a: MRI in lateral view. Large cystic craniopharyngioma in an adult with severe hormonal deficiency, drowsiness and visual deficit. The yellow arrow points to the small solid part, the red to the large cyst.
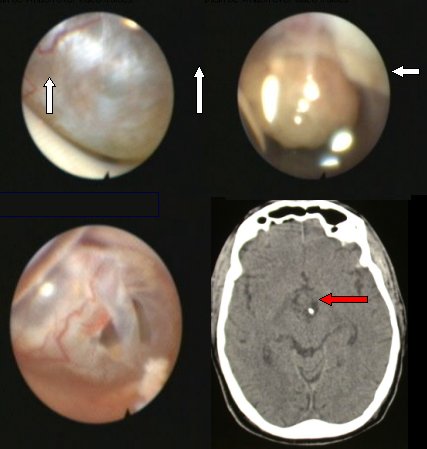
Fig.5.43b: From left to right: endoscopic images showing the cyst in the third ventricle and the perforated cyst. Bottom right: post-operative CT scan. The right arrow points to a microcatheter left in the cyst.
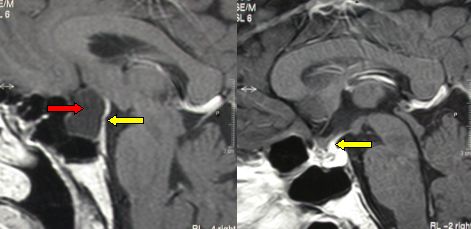
Fig.5.44: On the left, pre-operative lateral MRI of a Rhatke's cleft cyst. The red arrow points to the cyst, the yellow to the compressed and displaced pituitary stalk. On the right, post-operative view where stalk and pituitary gland have regained their normal position.
Page 21



 Glioma
Glioma Previous Page
Previous Page