Very large neurinomas may be frankly oligosymptomatic.
Contrast-enhanced CT scan and MRI are typical and the diagnosis is easy.
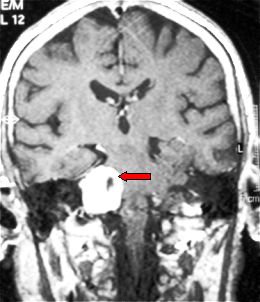
Fig. 5.35: Typical features of a right acoustic neurinoma, frontal MRI view (arrow).
As in the case of meningiomas, common-sense rules should be followed for neurinoma patients. Small remnants may be treated with radiosurgery or monitored over time with MRI or CT.
Radiosurgery may also be the treatment of choice for neurinomas smaller than 2.5 cm. The results reported in the latest literature are quite good.
They are benign tumors, similar to their intracranial counterparts. They are a little bit different in histology and may be called neurofibromas. They grow from the nerves within the spinal dura and outside the spinal cord: intradural extramedullary tumors. At times, they follow the nerve outside the spine in a dumbbell shape. They may be multiple. The most frequent location is in the lumbar spine, i.e. the neurofibroma takes origin from one of the nerves of the cauda equina.
Pain is the most frequent symptom; nocturnal pain, relieved in the upright position, is typical. If the spinal cord is compressed, there may be paraparesis or other senso-motor deficits, depending on the level of the lesion. Sphincteric disturbances may be present in large caudal neurofibromas.
Contrast-enhanced MRI is the tool for the diagnosis of spinal neurinomas.
The only therapy is microneurosurgical removal. Like in spinal meningioma, the mininvasive approach is relatively easy in experienced hands. Mininvasive neurosurgery shortens hospital stay, lowers costs, lessens the use of post-operative medication and eliminates the use of post-operative external devices and the risk of late spinal instability.

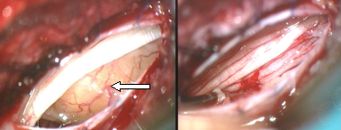
Fig.5.36: On the left, MRI picture of a spinal neurofibroma at L1 (red arrow); the yellow arrow points to the spinal cord. In the middle, the tumor as seen under the operating microscope, through a mininvasive approach; on the right, the "cauda equina" after tumor removal.
Page 19



 Glioma
Glioma Previous Page
Previous Page