This kind of tumor originates from the cells which line the
ventricular cavities of the
brain and the central canal of the
spinal cord (see
classification).
It is an infrequent brain tumor. It may occur in infancy and then it is mainly located in the posterior cranial fossa. In these cases, it is associated with hydrocephalus and
intracranial hypertension syndrome. "Complete" removal of a posterior cranial fossa
ependymoma is possible with modern intra-operative tools. If its biology is benign, there is no need for adjuvant radio-chemotherapy.
In adults,
ependymomas are mainly located in the lateral ventricles, where they grow and reach large volumes. Removal is not easy; both the surgery and the approach should be carefully investigated and planned to avoid damage to the healthy brain.

Fig.5.17: MRI image of an ependymoma of the left lateral ventricle (arrow).
Removal of a fourth ventricle ependymoma is technically less demanding; the implant on the floor of the ventricle may be coagulated with
laser or bipolar forceps. Radiotherapy on the implant may be necessary.
There are also malignant ependymomas that are aggressive. They must be treated with radio-chemotherapy after surgical removal.
Ependymomas of the
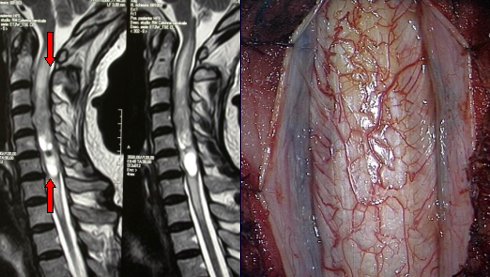
spinal cord are rather frequent: they originate from the ependymal cells of the central spinal canal or from the "filum terminalis", i.e. the most caudal part of the cord. This kind of tumors must be operated; "total" removal is generally possible, as they may be separated from the fibers of the spinal cord. There are also rare cases of ependymomas that extend along the whole cord (holocord ependymomas).

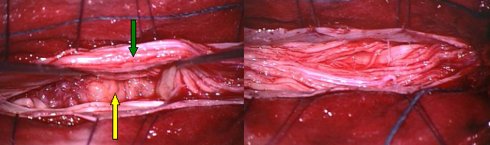
Fig.5.18a: MRI image of a large filum terminalis ependymoma (arrows).
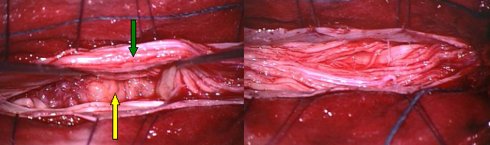
Fig.5.18b: Same case upon surgery. The yellow arrow points to the tumor; the green one to the spinal nerves of the cauda. On the right, the nerves after removal of the tumor.
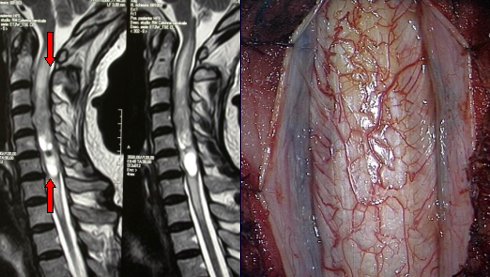
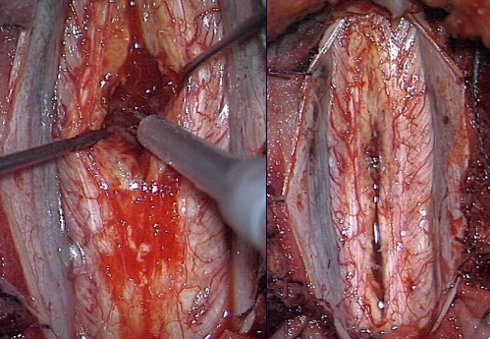
Fig.5.19: The upper left images show the MRI of an intramedullary cervical ependymoma (red arrows). Top right: the cervical spinal cord, as seen under the operating microscope. Bottom left: the tumor (purple) being removed with the ultrasonic aspirator. Bottom right: the cord after complete removal of this ependymoma.
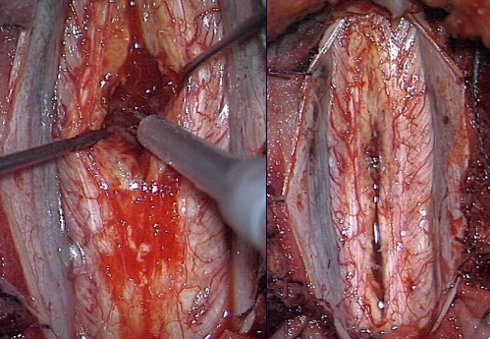
Primary brain lymphomas are not rare (0.5-2% of all brain tumors). They occur either in immuno-depressed patients (AIDS, after transplantation) or in normal population, where they are prevalent in elderly people. Primary brain lymphoma is classified as a non-Hodgkin one and derives from B lymphocytes.
It is a tumor of the
brain hemispheres,, generally with multiple locations. Diagnosis may be suspected on
MRI images.
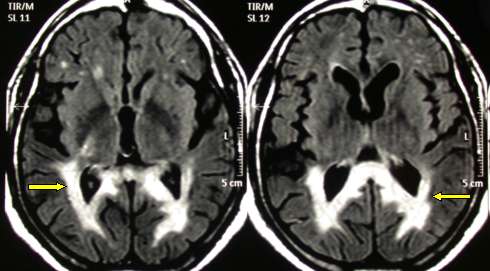
Fig.5.20: This is a quite typical MRI of a brain lymphoma. The arrows point to the periventricular pathological areas.
Stereotactic or frameless biopsy is mandatory to confirm diagnosis. Confusion with other pathologies (inflammatory, degenerative) may lead to a therapeutic disaster. Search of lymphomatous cells in the
cerebrospinal fluid (CSF) may be very useful.
Brain lymphomas often present with cognitive and psychic disturbances, which are typical in diffuse brain lesions.
intracranial hypertension, focal deficits and
seizures are also frequent.
The pathological images at
MRI or
CT may disappear after therapy with corticosteroids. In our opinion, this treatment should be avoided until diagnosis. Indeed, after treatment with corticosteroids, the target for the biopsy is no longer reliable.
Treatment may be resumed after biopsy and, if positive, high-dose chemotherapy and radiotherapy are indicated. Results are fair: some years of survival with good quality of life may be given to these patients.
Nevertheless, diffuse recurrences are the rule, also along the CSF pathways (i.e., malignant cells follow the CSF flow).
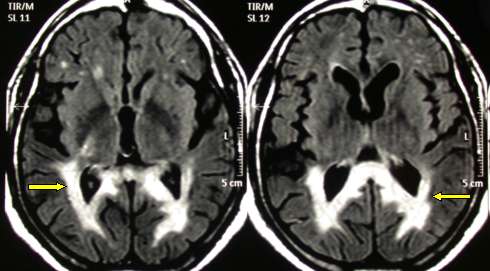
This tumor originates from the primitive, totipotential cells of the CNS. It is a malignant tumor, which generally affects children. It is located in the
cerebellum. Sometimes, it occurs in adults. It diffuses along the
CSF pathways.
Due to its cerebellar location, gait disturbances, hydrocephalus and
intracranial hypertension are the most frequent presenting symptoms.

Fig. 5.21: Left - MRI features of a medulloblastoma growing in the IV ventricle (red arrow). Right - the cavity after tumor removal (yellow arrow).
Surgery is the first step in treatment, possibly with gross total removal. Then, radiotherapy and chemotherapy are indicated, depending on stage of the tumor and age of the child (radiotherapy is contraindicated in early infancy). At present, thanks to appropriate and coordinated therapies, there are many long-term survivors among medulloblastoma patients. Good prognostic factors are gross total removal and absence of malignant cells in the CSF. Until the end of 1970s, the median survival was 12-24 months.






 Glioma
Glioma Previous Page
Previous Page