The pituitary is a small gland located at the base of the brain, in a bony pocket called "sella turcica". A dural tent separates it from the brain, with which it is connected via the pituitary stalk. The pituitary gland produces hormones that practically translate the orders of the brain to the benefit of other glands of the body: thyroid, sexual, mammalian, adrenal glands. It also releases the Growth Hormone, which acts directly on its targets.
Pituitary adenomas are primarily distinguished into hormone-producing or non-hormone-producing. The difference is crucial, as the former cause an endocrinological syndrome due to hormone hyperproduction, while the latter may cause hypofunction of the pituitary and, then, of the entire endocrinological system. In large producing adenomas, both conditions may occur. Non-producing adenomas are generally larger, as the diagnosis is done later. Thus, they often have a mass effect on the surrounding structures: optic nerves, optic chiasm, stalk, possibly brain. Pituitary adenomas are surgically classified according to their size: microadenomas (<1 cm), macroadenomas (1-2.5 cm), giant adenomas (>2.5 cm).
Another classification defines them as intrasellar, suprasellar and giant adenomas.
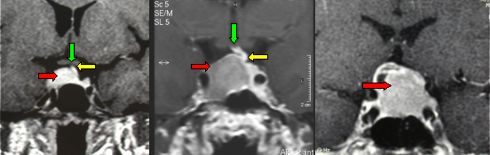
Fig.5.37: 3 cases of pituitary adenoma, as seen at frontal MRI. From left to right: 0.9 cm, 2 cm, 2.5 cm in diameter. The red arrows point to the adenomatous tissue, the green ones to the chiasm of the optic nerves and the yellow ones to the pituitary stalk. In the largest lesion, both chiasm and stalk are no longer detectable.
PRL-secreting adenomas cause infertility in females and impotence in males. When large enough, they bring about major pituitary insufficiency (panhypopituitarism). PRL adenomas may be invasive in the bone of the cranial base. Medical therapy with Cabergoline (an antiprolactinemic drug) may be very effective either in reducing hormone levels or the mass effect. If they are associated with visual deficits, surgical decompression may be indicated as the first step.
GH-secreting adenomas cause a medical syndrome called "acromegaly", which means that the extremities grow in an abnormal way: hands, feet, lips, supraorbital rims, tongue. These patients frequently develop diabetes and cardiopathy and are more exposed to tumors of the gastrointestinal tract. For GH adenomas, medical therapy based on somatostatin analogs is available. It is less effective and more expensive than the one for PRL adenomas. GH adenomas that are suitable for radical resection should probably be operated upon. In the other ones, mass reduction is anyway useful as a first therapeutic step. In cases with visual deficits due to chiasmal compression, surgery is mandatory. The visual recovery is generally excellent.
ACTH-secreting adenomas cause a severe illness, called Cushing's disease, which is characterized by arterial hypertension, cardiopathy, severe osteoporosis, obesity, severe diabetes, hypertricosis. There is no effective medical treatment. The therapy of choice is microneurosurgery.
Non-secreting adenomas cause a compressive damage to the pituitary gland. When large enough, they compress the optic chiasm from below. They should be operated upon.
Operation for pituitary adenoma is currently done through the transnasal-transphenoidal approach. We use the direct transnasal approach, assisted by the endoscope. Others use the pure endoscopic approach (see Chapter 7). The operation is performed under the surgical microscope, then also the endoscope is inserted. The direct transnasal route avoids all the complications that are secondary to nasal dissection and that are encountered with the sublabial and transeptal approaches. A retractor is inserted directly into the sphenoidal sinus.
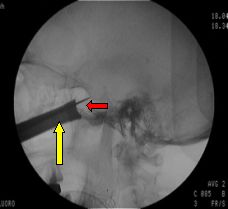
Fig.5.38: Intra-operative radioscopy with the inserted retractor (yellow arrow) and the microchisel on the sella turcica (red arrow). Afterwards, the sella is opened with a microrongeur or a microdrill; the dura is opened; and the adenoma (usually soft) is removed by suction and dissection.

Fig.5.39: Operative endoscopic view after pituitary adenoma removal.
The neuronavigator may be useful in very large adenomas, to define the boundaries of the tumor and the position of the carotid arteries.
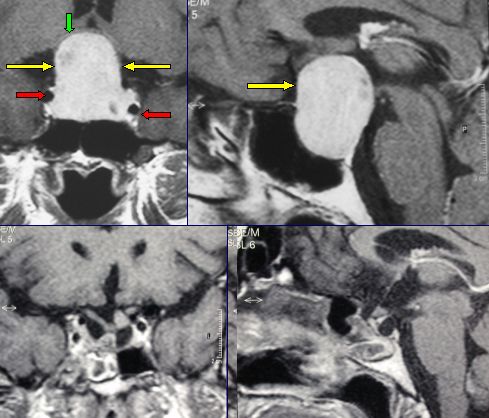
Fig.5.40: Frontal and lateral MRI views of a giant non-secreting pituitary adenoma. The green arrow points to the compressed and displaced chiasm, the yellow ones to the tumor and the red ones to the carotid arteries. Bottom: post-operative picture with total removal. This patient regained her normal vision.
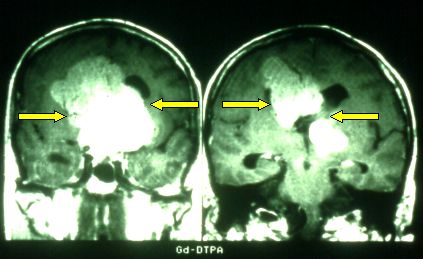
Fig.5.41: Monstrous adenoma ( > 8 cm ) in a comatous patient with severe panhypopituitarism who did not survive.
Actually, in expert hands and with modern operative technologies, results are very good.
The transcranial approach (subfrontal, pterional) is confined to very particular cases of pituitary adenomas.
Hormone replacement therapy, possibly decided by the endocrinologist, is very important either in the pre-operative days or in the post-operative period.
Adenomas are benign, slow-growing intracranial tumors. Generally, there is no reason to risk important functions to achieve total removal of adenomas that grow into the cavernous sinus or embed the carotid artery. The residual tumor may be monitored over time and/or treated with radiosurgery.
There are extremely rare cases of malignant adenomas: adenocarcinomas of the pituitary.
Also very rare are metastases to the pituitary from tumors in other sites. In the Author's series of more than 900 pituitary tumors, there are 7 of these cases.
Page 20



 Glioma
Glioma Previous Page
Previous Page