· Neurinomas
· Pituitary Adenomas
· Craniopharyngiomas
· Epidermoids
· Angiomas
· Chordomas, Chondromas, Chondrosarcomas
· Osteomas
· Metastases, that is all those brain tumors that arise from dissemination of cancers originating in other sites (lung, breast, melanoma, gastrointestinal tract, genitourinary tract).
This tumor originates from the arachnoid cells and extends to the dura. It is a connectival tumor, like a fibroma. Meningioma is an extraxial tumor; it occupies volume inside the skull or spine, but does not invade the nervous tissue, which is merely compressed and displaced. This does not mean that the nervous tissue does not suffer from the presence of the meningioma. It may activate compensation mechanisms for a long time, but when this compensation fails, the symptoms are severe and rapidly worsening.
Meningioma is a frequent tumor (27% of brain tumors) and more frequent in females. Those growing in the cerebral hemisphere are some more frequent, although they are ubiquitary in the intracranial space. Those of the vault are easy to remove, as they just lie on the cerebral cortex. Those of the cranial base need a deep trajectory to be reached; thus, some normal brain manipulation is needed to remove them.
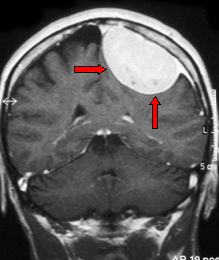
Fig. 5.28: Frontal view at MRI of a typical convexity meningioma.
There are also giant meningiomas that have scarce symptoms. This is due to the ability of the brain to live and work together with a slow-growing mass.
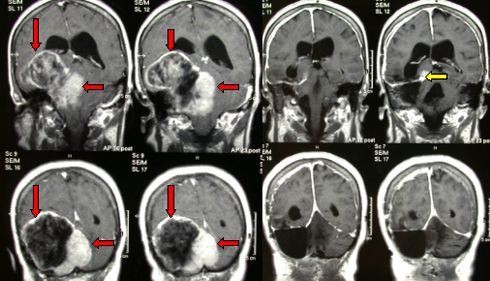
Fig.5.29a: This MRI in frontal view shows a giant meningioma (about 10 cm) that occupies 1/5 of the intracranial space (red arrows). On the right, the post-operative MRI. There is a small remnant (yellow arrow) that is irrelevant for the life of this patient.
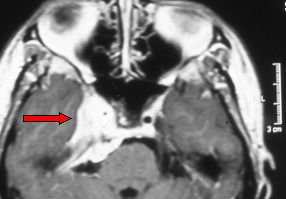
Fig.5.29b: The so-called sphenocavernous meningioma (arrow) in an axial MRI view. This tumor may rarely be removed without some damage to the oculomotor nerves and/or with a dangerous manipulation of the internal carotid artery. For this kind of meningioma, the indication is clinical observation and/or radiosurgery, as its volume is of less than 5 cc.
Total removal is obviously the goal. Microneurosurgical techniques make it possible to perform major and elegant operations by manipulating the brain through the natural corridors represented by the CSF cisterns. The neuronavigator may be useful. See Figures 6.4 and 6.5.
Total removal may be achieved also with mininvasive approaches. Mininvasive neurosurgery permits to remove fairly large meningiomas of the anterior cranial base through a small supraorbital approach.
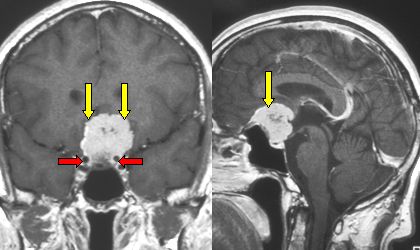
Fig. 5.30a: Frontal and lateral MRI views of a cranial base meningioma, tuberculum sellae meningioma (yellow arrows), adjacent to internal carotid arteries (red arrows), with severe optic nerve stretching and damage. This meningioma was removed with a mininvasive approach.
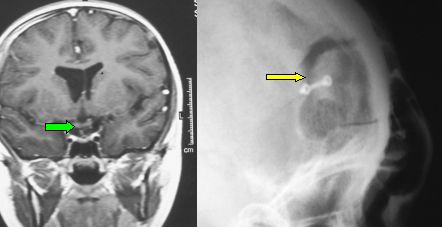
Fig.5.30b: This frontal MRI shows the complete removal without any cerebral contusion. The green arrow points to the optic chiasm that has returned to its normal position. On the right, a plain radiograph showing the small supraorbital flap.
The clinical symptoms of meningiomas depend on the volume and site of the tumor. Those of the convexity may present with seizures and hemiparesis, those of the anterior cranial base may be very large and cause severe intracranial hypertension, those of the cranial base may cause visual deficits, double vision, deficits of the lower cranial nerves.
Meningiomas may be occasionally found at CT scan or MRI that are done for other reasons. In these cases, the surgical indication must take in account the age and conditions of the individual patient. There are no definitive rules. It should be kept in mind that meningiomas are generally slow-growing tumors.
Meningiomas are evident at contrast-enhanced CT scan and MRI. The anatomical details are more evident at MRI. Angiographic MRI is useful to show their relationships with arteries and veins. Meningiomas may be partly calcified, thus they are visible also on a simple radiograph.
90% of meningiomas are benign. Nevertheless some of them cause suffering of the surrounding, compressed, brain tissue: edema. This edema is evident at MRI; it is the expression of the biological activity of the tumor. Meningiomas with edema present frequently with seizures.
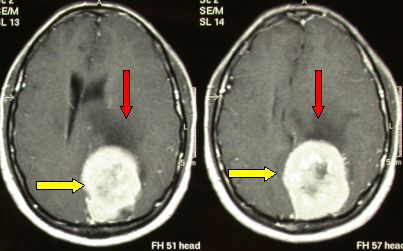
Fig.5.31: Axial MRI view of a large left parietal meningioma (yellow arrows) with clear brain edema (red arrows) and surrounding brain suffering and displacement.
There are also cases with multiple meningiomas: meningiomatosis. In these patients, the symptomatic one must be removed. The others may be monitored over time via serial CT or MRI.
Some meningiomas invade the bone of the skull with a minimal meningeal part: "en plaque meningioma". The main part of this kind of tumor is in the bone, the meningeal intracranial part is a diffuse carpet of tissue.
The operation is difficult, as these tumors are frequently in contact with vital arteries and nerves of the cranial base; bone demolition is significant and needs reconstruction.
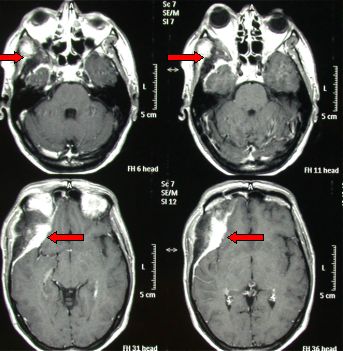
Fig.5.32: This axial MRI shows a typical right sphenorbital en plaque meningioma (red arrows). The right eye is pushed forward by the tumoral bony tissue.
Also benign meningiomas may recur, if the implant has not been completely removed upon surgery. This event is not rare in tumors located at the cranial base. Then, post-operative radiosurgery may be indicated.
Spinal meningiomas are rather rare. They are prevalent in females. Unlike spinal gliomas or ependymomas, they grow inside the dura but outside the spinal cord, which is compressed and displaced. They present with spinal pain and progressive neurological deficit below the level of the tumor. Symptoms may be severe; the spinal canal is a narrow space and the compensation is less easy than in brain meningiomas. MRI is the most useful diagnostic tool.

Fig.5.33: Lateral MRI view of a meningioma of the 5th dorsal segment (arrow) that compresses the spinal cord.
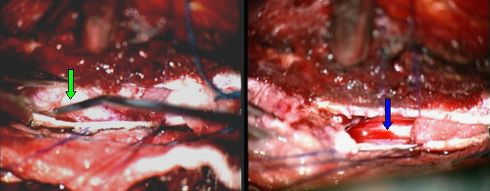
Fig.5.34: Operative view of the same case as in Fig. 5.37. The tumor (2.5 cm) is exposed (green arrow) through a "mini" window in the spine. On the right, the spinal cord after meningioma removal (blue arrow).
Page 18



 Glioma
Glioma Previous Page
Previous Page